Information & Resources for Workplaces- Coronavirus (COVID-19)
The 2019 novel coronavirus or SARS-CoV-2 is a new respiratory virus that has not been identified before; and thus people have no immunity to it. The virus causes diseases of varying severities ranging from mild (e.g. similar to common cold) to severe (e.g. pneumonia).
To obtain easy-to-read, question-and-answer fact sheets covering a wide range of COVID-19 workplace health and safety topics, click on one of the fact sheet topics below. In addition, easy to read posters issued by NIOH are available also below. All files are print ready, available in PDF format and can be used for awareness and education purposes.
Click here to view other NIOH resources such as: Cleaning guidelines for workplaces; COVID-19 Procedure for access for visitors; and the COVID-19 Self-declaration entry form. All other National Resources and Guidelines can be viewed here.
Frequently Asked Questions (FAQs)
A: No! Importantly no person can be forced to be vaccinated as per the President’s declaration. Individuals cannot be discriminated against in South Africa for not having the SARS-CoV2 vaccine.
A: A number of individuals who have had the disease have become re-infected. In some cases, infection does not result in significant immunity. In addition, there are variants of the disease circulating in South Africa so it is important to be vaccinated even if you had the infection previously. Similarly, there are cases of breakthrough infection even in vaccinated people especially with the variants. For that reason, vaccination does not mean that you are 100% protected. Importantly, vaccination significantly reduces the risk of severe disease and death.
A: Importantly, a number of individuals have had an antibody test after the vaccination. A reminder that serology (antibody tests) often measure antibodies against the nucleocapsid antigen and not against the spike antigen. This means that these tests will not pick up antibodies in people who have not had so-called “natural infection”.
A: If a number of individuals in a population have received a vaccine, they become immune and will not transmit the infection. This is generally considered to be about 2/3s of the population. This means that these individuals will protect other individuals in the population who cannot receive the vaccine for any reason.
A: The vaccine is currently not recommended for children under the age of 16 years. Children are also less likely to have severe disease. There has been some data that elderly patients may not respond as well to the vaccine but in South Africa, there is intention to vaccinate elderly patients who are at risk of severe disease and death.
A: Some preliminary data suggests that this may be the case although the vaccine suppliers suggest that there are limited efficacy data on this approach. It has been utilised in some countries however including the United Kingdom.
There is currently no certainty since the majority of the vaccines only have about 6 months of data. It may be necessary to have this vaccine more than once?
A: We are currently not sure since the majority of the vaccines only have about 6 months of data. It may be necessary to have this vaccine more than once?
A: If you are pregnant or breastfeeding
If you have a condition that effects the immune system e.g. if you have HIV or cancer
If you have had an allergic response in the past to vaccination
If you are susceptible to bleeding
If you have any symptoms of active SARS-CoV2 infection or a fever
If you have received another vaccine for SARS-CoV2
A: A number of individuals are on drugs which may suppress the immune response. This includes corticosteroids. Although there is no current indication that this affects the efficacy of the vaccine this remains something to monitor. Currently, pain medication (like non-steroidal anti-inflammatory drugs) are being used in vaccinated individuals who present with side-effects like injection site pain.
A: There is limited data available on the effect on pregnancy. Most vaccines have, however, been effective in pregnant women. Because of the risk of severe SARS-CoV2 infection in pregnant women, the WHO has recently reversed its decision not to recommend vaccination of pregnant women and many countries are now actively vaccinating women in the 2nd and 3rd trimester (www.who.int)
A: Clotting is increased in individuals who are inflamed and for this reason any immunological challenge may increase the risk of clotting (including the vaccine) however, the risk of clotting does not appear very high and the risk of abnormal clots with severe COVID-19 are very high indeed. It is therefore better to take the vaccine risk than the risk of severe disease.
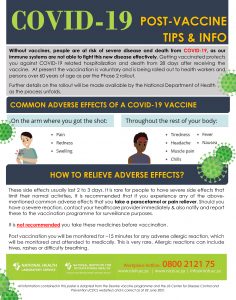
A: These vaccines are designed to activate the immune system. This can produce temporary side effects. This includes injection site pain, low grade fever, rash, muscle aches. In the large scale studies, these were reported by the participants generally as mild and lasted for a few days only. There have been reports of severe allergic responses to some but not all vaccines. These are extremely uncommon (approximately 0.001% of participants) and have not be conclusively linked to the vaccine. Importantly, side-effects are more likely to occur after the second dose of the vaccine.
A: No. Some viruses, retroviruses like HIV, are inserted into the host genetic material and can cause mutations. The genetic material of SARS-CoV2 is not inserted and the vaccines will also not result in genetic manipulation.